Understanding the Skin Microbiome and its Relationship to Dermal Therapies

Image Source - wellnessbyrosh.com
This information is intended for Dermal Therapists and Cosmetic Nurses or anyone considering completing a formal course in dermal science or a cosmetic nursing course.
Introduction
The human body contains trillions of microorganisms out numbering our human cells by 10 to one. In fact, microorganisms make up only about 1-3% of the body’s mass and this is inclusive of both the internal and external microorganisms that we live with, and that call us home.
According to Skowron et al. (2021), the average surface area in an adult of 30 m2 and a thickness of 2-3mm, our outer barrier, our skin. Eyerich et al. (2018) suggest that it is a highly interconnected network of cells that provides protection against environmental factors, acts as an immunological barrier, helps regulate body temperature by preventing water loss, enabling temperature sensation and the synthesis of vitamin D when exposed to UV light,
For our skin to accomplish all these functions and more intrinsically the skin requires a diverse and large array of microbiome that interact via the gut-skin axis. The gut and the skin are two primary locations that need protection and it is no coincidence that they are intimately connected.
So important is our need to understand this connection that in 2007, in the US launched, “The Human Microbiome Project”, with the goal to develop research resources that would enable researchers to study the microbial communities that live in and on our bodies and the roles they play in human health and disease. Prior to the start of the Human Microbiome Project, this abundant community of human-associated microbes remained largely unstudied and ignored, leaving their influence on our human development, physiology, immunity, and nutrition to be almost entirely unknown. However, to date, there have been over 650 scientific papers that had been cited over 70,000 times (Mahmud et al., 2022).
Skin microbiome composition at different stages
Casterline and Paller (2021) suggest that the placental microbiome may influence the metabolism and immune response of the foetus, as metagenomic sequencing has revealed a rich placental microbiome in healthy pregnancies that is likely to influence the developing metabolic and immune responses of the foetus. While there has been a focus on the gut microbiome and how it may colonise and affect the health of the skin, after birth, microbe acquisition is known to be influenced by multiple factors such as the mode of delivery, (Vaginal or Caesarean), breast fed or formulae fed infants, antibiotics and ahigh processed, high fat, low fiber diet (Kemter & Nagler, 2019).
Microorganisms isolated from various parts of the body of a newborn who were a natural delivery belong to the maternal genius Lactobacillus, Prevotella and Sneathia. In turn a newborn child born Cesarean section’s skin microbiota mostly was shown to consist of staphylococcus, Cornebacterium and Cutibacterium.
The relationship the newborn has with its mother, influences the transmission of microorganisms between them as does environmental factors that increase the species diversity on the skin. By the time the child is one the dominance of bacteria belongs to the firmicutes type followed by Actinobacteria and bacteroides. Diversity of the skin microbiome progresses until the age of eight. In adults Bacteriodes phyla are the most common followed by Actinobacteria, Proteobacteria and Firmicutes. However the skin site and its characteristic does determine the prevalent species (Grice & Segre, 2011), see diagram below.
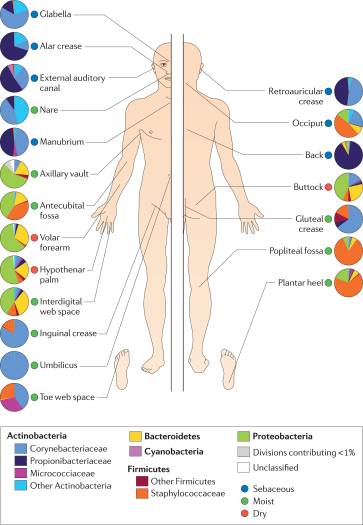
Source: (Grice & Segre, 2011)
Gut-skin axis and its microbiota composition
Our skin shelters numerous commensal microbes (bacteria, fungi and viruses) and can be broadly categorized as sebaceous or oily (glabella), moist (antecubital fossa) or dry (volar forearm), according to the physiological characteristics of each skin site (Eyerich et al., 2018). Specific microbial communities dominate different skin sites. Please see the diagram below.
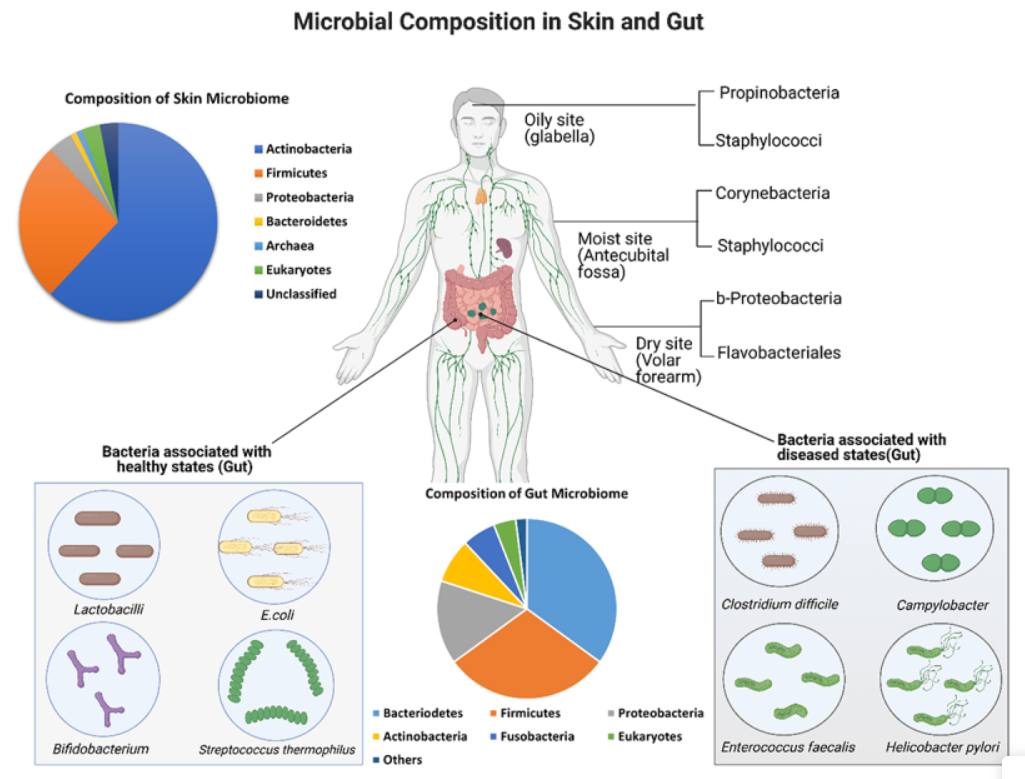
Source: (Mahmud et al., 2022)
The skin’s front-line defence, the epidermal layer, includes multiple heterogenous layers and they each preform a specialise role. Like other barriers in the body the cutaneous barrier consists of microbial, immune, chemical, and physical components. Gut-skin communication occurs through the activities of immunological components which are present between the gut and the skin.
Whilst the mechanism and triggers are not fully clear, research has demonstrates that there is an undisputable link between the microbiome, the immune system and the skin. When the immune system is impaired the domino effects can trigger the development of skin diseases.
Several dermatologic conditions, such as acne, atopic dermatitis, psoriasis, and rosacea are linked with intestinal dysbiosis and many studies have associated gastrointestinal health with skin homeostasis and allostasis (Grice & Segre, 2011; Kemter & Nagler, 2019; Mahmud et al., 2022).
There is evidence of a bidirectional inter-action between the gut and the skin, just as there is with the brain and the gut and according to (Mahmud et al., 2022).
“the gut skin communication occurs through the activities of immunological components which are present between the gut and the skin.” Para.13
Members of the gut microbiome can influence skin health and function through their metabolic activity and immunological impact. For example, commensal gut microbes can foster skin allostasis by controlling T-cell differentiation. According to (Campbell et al., 2017), Skin commensal microbiome can also be affected by bioactive compounds such as neurotransmitters, hormones and short chain fatty acids (SCFA’S), by inhibiting the growth of pathogenic microbes such as S. aureua (Ohkubo et al., 2022), which are the end products of gut microbial metabolism and maintain healthy fact. Campbell et al. (2017) suggests that even emotions may have the ability to influence skin barrier structure and human health.
Preserving a health skin barrier
The skin’s outer most lipid layer the stratum corneum safeguards the skin from desiccation by forming an impermeable barrier and provides a substrate for the skin’s microbiota to interact.
The generation of free fatty acids on the surface of the skin creates a low pH environment (pH 4-6), which is essential for barrier homeostasis (Smythe & Wilkinson, 2023). A low pH is essential for supporting lipid substrate production, maintaining hydration levels and conserving the commensal skin microflora.
When diverse and physiologically established the skin’s microbiota or flora is instrumental as the body’s first line of defence. The commensal skin microbiota protects from pathogens and helps maintain the immune system’s delicate barrier between effective protection and damaging inflammation, For example, Commensal bacteria such as Staphylococcus epidermidis produce antimicrobial substances that fight off pathogens, whereas Cutibacterium acnes uses skin lipids to make short chain fatty acids assist in fighting bacterial threats (Smythe & Wilkinson, 2023).
The diversity of healthy skin microbiota is higher in the younger population than adults and sharply different between the two age groups. An example of these commensals would be Streptococcus Rothias, Gemella, Granulicatella and Haemophilus are present in young children while Cutibacterium, Lactobacillus, Anaerococcus, Finegoldia and Corynebacterium are more common on the skin of adults as normal flora.
Nine strategies to promote the health and integrity of the microbial communities of the skin
There is much to learn about the gut – skin axis and their microbial species that support normal flora however until we fully master and understand more information coming through from future researcher the main traits of a healthy skin microbiome that persevere the largest organ of our body are:
- Nurture gut health which will in turn nurture skin health.
- Whenever possible a newborn should be naturally delivered and breast feed thereby positively influencing further natural gut and skin microbiome diversity.
- A diet rich in fibre support gut microbiome and the manufacturing of SCFA beneficial to both gut mucosa health and function. For the skin SCFA have an anti-inflammatory effects and have been shown to reduce skin inflammation via the immune system bidirectional pathway (Ohkubo et al., 2022).
- Use antibiotics sparingly, due to their impact on the loss of keystone microbial species and diversity. For example, an overgrowth of Candida due to antibiotic use can colonise the small intestine and manifest symptoms as skin redness, which in turn accelerates aging.
- Avoid toxic environments and personal care products such as hair dye that contain a high ammonia content.
- Support gut microbial health through nutrient dense food and food that has not been modified such as highly processed foods.
- Avoid use of harsh skin cleansers and treatments that impact and later the skin’s natural pH (Lambers et al., 2006).
- Consider the use of nutraceuticals such as prebiotics and probiotics. For example, Lactobacillus reuteri, has been shown to improve epidermal thickness and collagen deposition (Mahmud et al., 2022).
- Keep the gut and skin hydrated to ensure ease of detoxification and elimination of waste material.
Want to know more?
If you’re loving anything and everything about the skin and health, you can enrol in the following courses:
Graduate Diploma of Cosmetic Nursing and Injectables (nationally recognised qualification)
Graduate Diploma of Dermal Science (nationally recognised qualification)
Professional Certificate in Integrated Health and Dermatology (16-week course)
References:
Campbell, D., Burks, W., Caraballo, L., Horwitz, P., Kozyrskyj, A., Larcombe, D.-L., Levin, M., Logan, A., Prescott, S., & Van Etten, E. (2017).
The skin microbiome: Impact of modern environments on skin ecology, barrier integrity, and systemic immune programming.
Casterline, B. W., & Paller, A. S. (2021). Early development of the skin microbiome: therapeutic opportunities. Pediatric research, 90(4), 731-737.
Eyerich, S., Eyerich, K., Traidl-Hoffmann, C., & Biedermann, T. (2018). Cutaneous barriers and skin immunity: differentiating a connected
network. Trends in immunology, 39(4), 315-327.
Grice, E. A., & Segre, J. A. (2011). The skin microbiome. Nature Reviews Microbiology, 9(4), 244-253.
Kemter, A. M., & Nagler, C. R. (2019). Influences on allergic mechanisms through gut, lung, and skin microbiome exposures. The Journal of
clinical investigation, 129(4), 1483-1492.
Lambers, H., Piessens, S., Bloem, A., Pronk, H., & Finkel, P. (2006). Natural skin surface pH is on average below 5, which is beneficial for its
resident flora. International journal of cosmetic science, 28(5), 359-370.
Mahmud, M. R., Akter, S., Tamanna, S. K., Mazumder, L., Esti, I. Z., Banerjee, S., Akter, S., Hasan, M. R., Acharjee, M., & Hossain, M. S. (2022).
Impact of gut microbiome on skin health: gut-skin axis observed through the lenses of therapeutics and skin diseases. Gut Microbes, 14(1),
2096995.
Ohkubo, T., Matsumoto, Y., Ogasawara, Y., & Sugita, T. (2022). Alkaline stress inhibits the growth of Staphylococcus epidermidis by inducing TCA
cycle-triggered ROS production. Biochemical and Biophysical Research Communications, 588, 104-110.
Skowron, K., Bauza-Kaszewska, J., Kraszewska, Z., Wiktorczyk-Kapischke, N., Grudlewska-Buda, K., Kwiecińska-Piróg, J., Wałecka-Zacharska,
E., Radtke, L., & Gospodarek-Komkowska, E. (2021). Human skin microbiome: impact of intrinsic and extrinsic factors on skin microbiota.
Microorganisms, 9(3), 543.
Smythe, P., & Wilkinson, H. N. (2023). The skin microbiome: current landscape and future opportunities. International journal of molecular
sciences, 24(4), 3950.